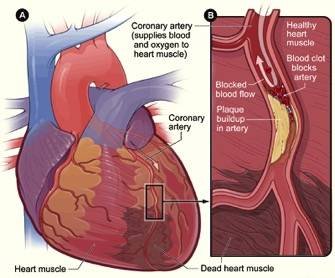
Acute coronary syndrome (ACS) represents a spectrum of clinical conditions caused by acute myocardial ischemia. The diagnostic process involves rapid identification and stratification based on clinical presentation, electrocardiography (ECG), and cardiac biomarkers. This article outlines the standard diagnostic approach employed in emergency settings, suitable for both academic citation and clinical instruction.
Introduction
Acute coronary syndrome encompasses a range of urgent cardiac events, including ST-elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI), and unstable angina. Prompt and accurate diagnosis in the emergency department (ED) is crucial to improving outcomes and initiating appropriate therapy. The diagnostic algorithm integrates clinical evaluation, ECG interpretation, and cardiac biomarker analysis.
Diagnostic Approach
1. Clinical Presentation
The initial assessment focuses on patient-reported symptoms. Classic manifestations include central chest pain or pressure, often radiating to the left arm, neck, or jaw. Symptoms may also include dyspnea, diaphoresis, nausea, or syncope. Importantly, atypical presentations are more common among elderly patients, women, and those with diabetes mellitus1
2. Electrocardiogram (ECG)
A 12-lead ECG is the first-line diagnostic test and should be performed within 10 minutes of ED arrival2. The presence of new ST-segment elevation in at least two contiguous leads, or a new left bundle branch block (LBBB), is diagnostic of STEMI. Such findings necessitate emergent reperfusion therapy—typically percutaneous coronary intervention (PCI) or, where unavailable, fibrinolytic therapy3.
If ST elevation is absent, serial ECGs are recommended to detect evolving changes that may suggest ongoing myocardial ischemia4.
3. Cardiac Biomarkers
Measurement of serum cardiac troponins (I or T) is essential for identifying myocardial injury. Elevated troponins confirm myocardial infarction, distinguishing NSTEMI from unstable angina, in which troponin levels remain normal despite ischemic symptoms5. Repeat testing is often required at 3- to 6-hour intervals to detect dynamic changes.
4. Risk Stratification and Monitoring
Patients diagnosed with NSTEMI or unstable angina are typically admitted to a coronary care unit (CCU) for telemetry and continuous observation. Risk assessment tools, such as the TIMI and GRACE scores, are used to guide the urgency of further diagnostic or interventional strategies6.
5. Further Evaluation
Following stabilization, patients may undergo non-invasive or invasive testing:
- Stress testing (exercise or pharmacologic) evaluates inducible ischemia in patients with intermediate risk.
- Coronary angiography is indicated for high-risk patients and allows for definitive identification and treatment of obstructive coronary lesions7.
Conclusion
The diagnostic process for acute coronary syndrome is multi-tiered and time-sensitive. It involves clinical judgment, ECG analysis, and biomarker evaluation, often supplemented by risk stratification and imaging. Timely differentiation among STEMI, NSTEMI, and unstable angina directly impacts therapeutic strategy and patient prognosis. This approach reflects current best practices in emergency cardiology and forms the basis for clinical decision-making globally.
To learn more usmle step 2 knowledge, tips, and strategies visit the main page
Footnotes
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes. Circulation. 2014;130(25):e344-e426.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39(2):119-177.
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2013;61(4):e78-e140.
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2016;37(3):267-315.
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction. Circulation. 2018;138(20):e618-e651.
- Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ. 2006;333(7578):1091.